Identification of novel bacterial virulence factors and inflammation determinants associated with persistent lung infections in Cystic Fibrosis
2020 – 2024
Overview
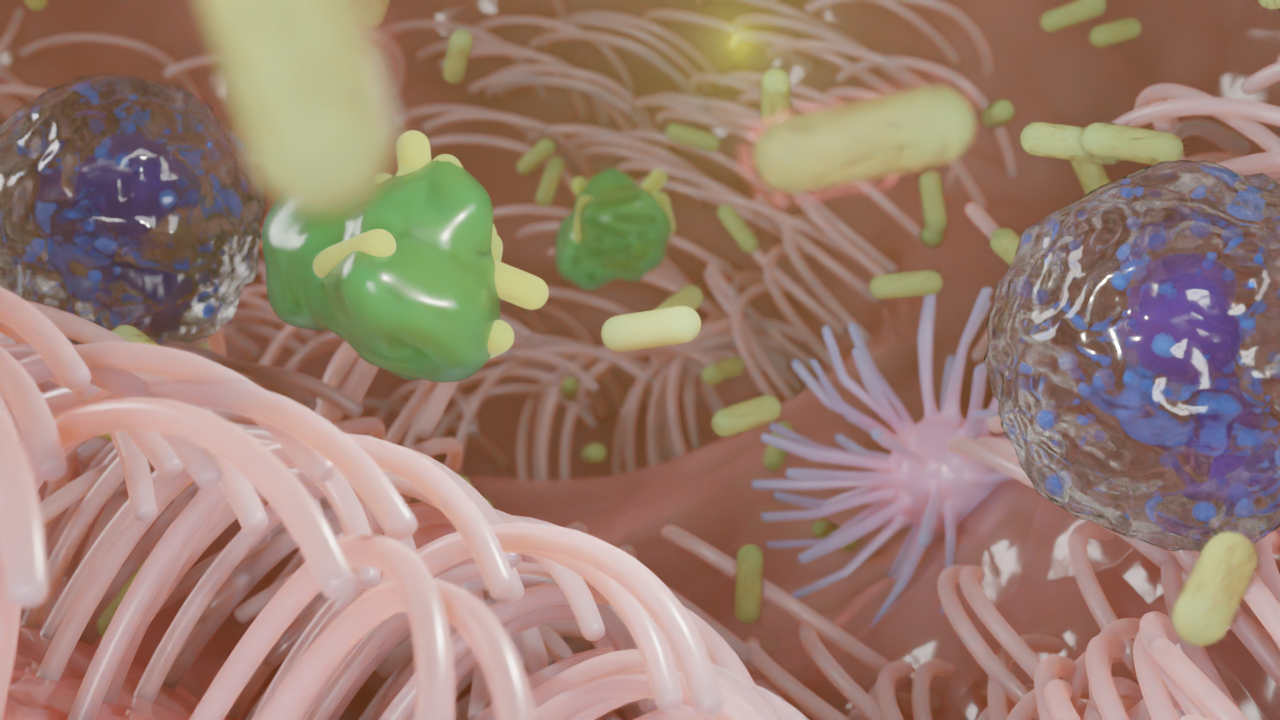
Chronic lung infections caused by Pseudomonas aeruginosa are a leading cause of mortality and reduced quality of life in cystic fibrosis (CF) patients. Despite advances in medical treatment, eradicating this pathogen remains a significant challenge. This innovative research project, generously funded by Fondazione Cariplo, focuses on uncovering the molecular and physiological mechanisms that enable P. aeruginosa to persist in the hostile environment of CF airways, drive inflammation, and evade host defenses. By bridging cutting-edge molecular biology, advanced infection models, and translational approaches, the project aims to redefine treatment strategies for CF-associated infections.
Aims
This research strives to:
- Decipher Pathogenic Mechanisms: Identify and characterize the genetic and metabolic pathways that support P. aeruginosa persistence in the unique environment of CF airways.
- Understand Host-Pathogen Interactions: Explore how P. aeruginosa interacts with the host’s immune system to sustain chronic infections and provoke an exaggerated inflammatory response.
- Develop New Therapeutic Strategies: Use insights from the research to identify novel molecular targets for therapies aimed at reducing bacterial persistence and inflammation.
- Advance Experimental Models: Establish robust infection models using human-derived airway organoids that closely mimic CF conditions.
Why This Project Matters?
Despite decades of research, P. aeruginosa infections in CF remain resistant to eradication, primarily due to gaps in understanding the pathogen’s physiology in vivo. This project bridges these gaps by:
- Targeting the actual processes occurring in CF airways, rather than relying solely on in vitro models.
- Shedding light on the paradoxical inflammatory responses triggered by less virulent bacterial forms.
- Offering translational solutions that can be quickly adapted to clinical practice, including drug development and diagnostic tools.
Methods
To achieve its goals, the project employs a comprehensive and interdisciplinary approach:
- Gene Expression Profiling:
- Using transcriptomics, the project investigates P. aeruginosa gene expression directly in patient-derived sputum samples to capture real-time bacterial responses in vivo.
- Identification of differentially expressed genes (DEGs) that regulate persistence and immune evasion.
- Mutant Strain Library:
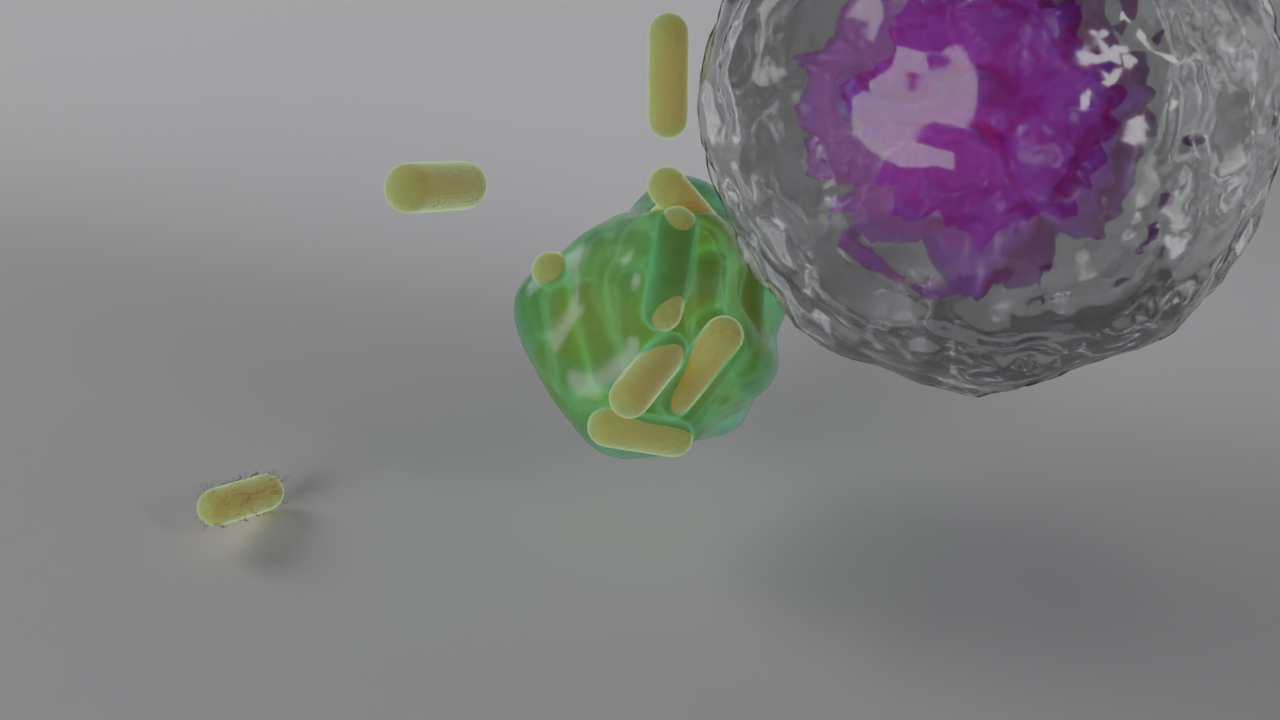
- A library of P. aeruginosa knockout (KO) and overexpression (OEXP) mutants is created to test their roles in biofilm formation, stress resistance, and virulence.
- RNA sequencing is performed on these mutants to uncover system-wide physiological changes and regulatory networks.
- Human Airway Organoids:
- Patient-derived human airway organoids (HAOs) are used to replicate CF airway conditions. These three-dimensional models provide insights into colonization, tissue damage, and immune response.
- Organoids are infected with mutant strains to evaluate bacterial persistence, inflammatory response, and neutrophil recruitment.
- Collaborative Framework:
- The project benefits from the expertise of two research units: the University of Milan, Italy, and Rigshospitalet, Copenhagen, Denmark. This collaboration ensures a combination of molecular techniques and advanced infection models.
- Advanced Imaging Techniques:
- Confocal microscopy and time-lapse imaging are utilized to visualize bacterial colonization and immune cell recruitment in organoid models, offering dynamic insights into host-pathogen interactions.
- Data Analysis and Validation:
- A robust statistical framework and machine learning algorithms are applied to analyze complex datasets, ensuring reproducibility and reliability of findings.
Expected Outcomes
Scientific Impact:
- PaEnhanced Understanding: Gain a deeper knowledge of the metabolic and genetic adaptations of P. aeruginosa in CF airways.
- Target Identification: Identify key molecular pathways and genes that can serve as potential targets for therapeutic intervention.
- Model Development: Establish HAOs as a reliable and translatable model for studying CF-related infections.
Societal Relevance:
- Better Treatments: Provide a foundation for developing precision medicine approaches that target P. aeruginosa persistence mechanisms, improving outcomes for CF patients.
- Reduced Healthcare Burden: Alleviate the impact of chronic infections and associated inflammation on healthcare systems and patient quality of life.
- Public Awareness and Engagement: Through active dissemination efforts, educate patients, clinicians, and the broader public about advancements in CF treatment.
Partners
Fundings
Publications from the project
2024
-
![[DOI]](https://www.rossimicrolab.com/wp-content/plugins/papercite/img/external.png) E. Rossi, M. Lausen, N. F. Øbro, A. Colque, B. U. Nielsen, R. Møller, C. de Gier, A. Hald, M. Skov, T. Pressler, S. Molin, S. R. Ostrowski, H. V. Marquart, and H. K. Johansen, “Widespread alterations in systemic immune profile are linked to lung function heterogeneity and airway microbes in cystic fibrosis,” Journal of cystic fibrosis, 2024.
E. Rossi, M. Lausen, N. F. Øbro, A. Colque, B. U. Nielsen, R. Møller, C. de Gier, A. Hald, M. Skov, T. Pressler, S. Molin, S. R. Ostrowski, H. V. Marquart, and H. K. Johansen, “Widespread alterations in systemic immune profile are linked to lung function heterogeneity and airway microbes in cystic fibrosis,” Journal of cystic fibrosis, 2024.
[Bibtex]@article{Rossi.2024, year = {2024}, title = {{Widespread alterations in systemic immune profile are linked to lung function heterogeneity and airway microbes in cystic fibrosis}}, author = {Rossi, Elio and Lausen, Mads and Øbro, Nina Friesgaard and Colque, Antonella and Nielsen, Bibi Uhre and Møller, Rikke and Gier, Camilla de and Hald, Annemette and Skov, Marianne and Pressler, Tacjana and Molin, Søren and Ostrowski, Sisse Rye and Marquart, Hanne Vibeke and Johansen, Helle Krogh}, journal = {Journal of Cystic Fibrosis}, issn = {1569-1993}, doi = {10.1016/j.jcf.2024.04.015}, pmid = {38702223}, abstract = {{Background Excessive inflammation and recurrent airway infections characterize people with cystic fibrosis (pwCF), a disease with highly heterogeneous clinical outcomes. How the overall immune response is affected in pwCF, its relationships with the lung microbiome, and the source of clinical heterogeneity have not been fully elucidated. Methods Peripheral blood and sputum samples were collected from 28 pwCF and an age-matched control group. Systemic immune cell subsets and surface markers were quantified using multiparameter flow cytometry. Lung microbiome composition was reconstructed using metatranscriptomics on sputum samples, and microbial taxa were correlated to circulating immune cells and surface markers expression. Results In pwCF, we found a specific systemic immune profile characterized by widespread hyperactivation and altered frequencies of several subsets. These included substantial changes in B-cell subsets, enrichment of CD35+/CD49d+ neutrophils, and reduction in dendritic cells. Activation markers and checkpoint molecule expression levels differed from healthy subjects. CTLA-4 expression was increased in Tregs and, together with impaired B-cell subsets, correlated with patients' lung function. Concentrations and frequencies of key immune cells and marker expression correlated with the relative abundance of commensal and pathogenic bacteria in the lungs. Conclusion The CF-specific immune signature, involving hyperactivation, immune dysregulation with alteration in Treg homeostasis, and impaired B-cell function, is a potential source of lung function heterogeneity. The activity of specific microbes contributes to disrupting the balance of the immune response. Our data provide a unique foundation for identifying novel markers and immunomodulatory targets to develop the future of cystic fibrosis treatment and management.}}, local-url = {file://localhost/Users/elioros/Documents/Papers%20Library/Rossi-Widespread%20alterations%20in%20systemic%20immune%20profile%20are%20linked%20to%20lung%20function%20heterogeneity%20and%20airway%20microbes%20in%20cystic%20fibrosis-2024-Journal%20of%20Cystic%20Fibrosis.pdf} } -
![[DOI]](https://www.rossimicrolab.com/wp-content/plugins/papercite/img/external.png) R. Møller, B. U. Nielsen, E. Rossi, M. Lausen, M. Skov, T. Pressler, S. R. Ostrowski, and H. K. Johansen, “Clinical implications of innate immune exhaustion in cystic fibrosis,” Erj open research, vol. 10, iss. 4, p. 00256–2024, 2024.
R. Møller, B. U. Nielsen, E. Rossi, M. Lausen, M. Skov, T. Pressler, S. R. Ostrowski, and H. K. Johansen, “Clinical implications of innate immune exhaustion in cystic fibrosis,” Erj open research, vol. 10, iss. 4, p. 00256–2024, 2024.
[Bibtex]@article{Møller.2024, year = {2024}, title = {{Clinical implications of innate immune exhaustion in cystic fibrosis}}, author = {Møller, Rikke and Nielsen, Bibi Uhre and Rossi, Elio and Lausen, Mads and Skov, Marianne and Pressler, Tacjana and Ostrowski, Sisse Rye and Johansen, Helle Krogh}, journal = {ERJ Open Research}, issn = {2312-0541}, doi = {10.1183/23120541.00256-2024}, pmid = {39193378}, pmcid = {PMC11347999}, abstract = {{Lung disease progression in people with cystic fibrosis (pwCF) varies from one individual to another. Different immunological characteristics have been suggested to explain this variation, and we hypothesised that lung capacity may be associated with the innate immune response in pwCF. In an exploratory study, we aimed to investigate potential links between the innate immune response and lung function in pwCF using the standardised immune function assay TruCulture. In a single-centre study with combined cross-sectional and longitudinal data before and after intravenous antibiotics, blood was sampled from Pseudomonas aeruginosa-infected pwCF. Whole blood was analysed by TruCulture to reveal the unstimulated and stimulated cytokine release. Tobit regressions and Spearman's correlations were used to estimate the associations between lung function and cytokine release. We included 52 pwCF in the cross-sectional study and 24 in the longitudinal study. In the cross-sectional study, we found that compared to a healthy population, the release of toll-like receptor (TLR)3, TLR4- and TLR7/8-stimulated interferon-γ, and interleukin (IL)-12p40 was reduced. Although TLR3-stimulated IL-1β and IL-6 release increased with lung function, overall, cytokine release did not correlate well with lung function. In the longitudinal study, the cytokine release was modified by antibiotic treatment, but the cytokine release before antibiotic treatment did not associate with changes in lung function after treatment. The stimulated cytokine release could not predict lung function levels or changes in pwCF, but our data indicate that pwCF experience exhaustion in the innate immune response after years of chronic bacterial infection.}}, pages = {00256--2024}, number = {4}, volume = {10} }



